Toothache: Causes, Treatment and Prevention
A toothache can cause significant discomfort to you. It can even impede you from going about with your day normally. A toothache can also be the start of bigger dental and health problems.
Why does my tooth hurt?
If your tooth is feeling pain, it is most likely hurting because of the following reasons:
- Infected tooth pulp (pulpitis)
- Tooth decay (cavities)
- Damaged or missing dental fillings
- Teeth grinding (bruxism)
- The progression of gum disease
- Tooth fracture
- Tooth abscess
- Impacted wisdom tooth
What is a toothache?
A toothache is pain or discomfort in or around a tooth. It can range from mild to severe and may be constant or intermittent. Symptoms often include:
- Sharp, throbbing, or constant pain
- Sensitivity to hot or cold temperatures
- Pain when chewing or biting
- Swelling around the tooth
- Fever, headaches or migraines in severe cases
Toothaches can be indicators of serious dental issues and often require professional treatment. Taking an off-the-counter painkiller might help ease the pain but does not treat the root cause of the toothache.
If you have been experiencing persistent tooth pain, it is advisable to consult a dental clinic like Kong Dental Surgery for proper diagnosis and treatment.
Types of toothaches
There are several types of toothaches. Each of them potentially signals different underlying problems:
Sharp and sudden pain
- Often triggered by hot, cold, or sweet stimuli
- May indicate tooth decay, a loose filling, or exposed dentin
Dull and persistent ache
- Constant pain that may worsen with pressure
- Could be a sign of tooth grinding (bruxism) or an abscess
Throbbing pain
- Often accompanied by swelling
- May indicate an infection or abscess
Pain when biting or chewing
- Could be caused by a cracked tooth, loose filling, or decay
Sinus-related tooth pain
- Affects upper teeth on both sides
- Often associated with sinus congestion or infection
Gum pain
- Sore, tender gums
- May indicate gum disease or the emergence of wisdom teeth
Referred pain
- Pain that seems to come from the teeth but originates elsewhere
- Could be related to jaw problems, ear infections, or even heart issues
Wisdom tooth pain
- Often affects the back of the mouth
- May cause pain, swelling, and difficulty opening the mouth
Symptoms and Causes of Toothache
What causes a toothache?
A toothache can be caused by many different reasons. While dental cavities are the most frequent culprit behind toothaches, it is important to note that jaw pain can sometimes indicate more serious health issues. For instance, sinus infections can cause discomfort that mimics a toothache in the upper jaw. In rare cases, jaw pain may even be a symptom of a heart attack, though this is less common.
Tooth pain can range from a mild annoyance to an intense, debilitating sensation. It may manifest as a dull, persistent ache or a sharp, pulsating discomfort that interferes with everyday activities like eating, talking, and resting.
Toothaches vary in their intensity and duration, potentially disrupting your quality of life until the underlying cause is addressed. Given the diverse potential causes, it is crucial to seek professional dental evaluation for persistent or severe tooth pain to ensure proper diagnosis and treatment.
To provide further insight, the main causes of a toothache can be broken down into the following:
Tooth decay (cavities)
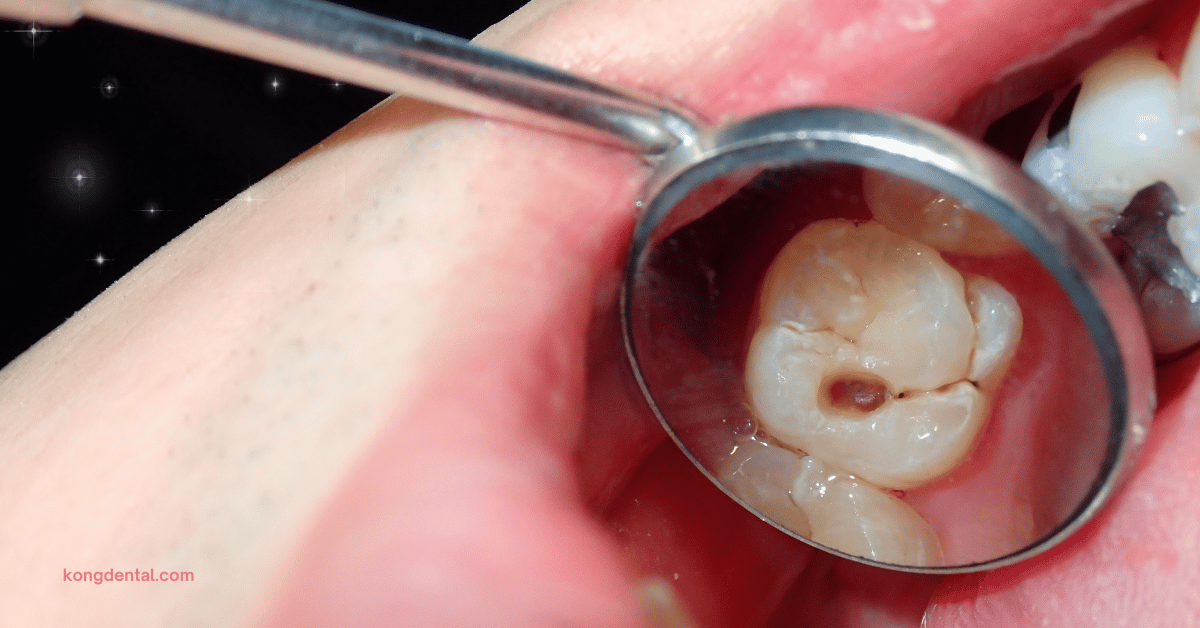
- Caused by bacteria that produce acid, eroding tooth enamel
- Decay can progress to deeper layers, causing pain when it reaches the dentin or pulp
- Often results from poor oral hygiene and high sugar consumption
Gum disease

- Begins as gingivitis (inflammation of the gums)
- Can progress to periodontitis, affecting the bone supporting the teeth
- Causes gum recession, exposing sensitive tooth roots
- Often results from poor oral hygiene and can be exacerbated by smoking
Tooth fracture (cracked tooth)

- Can be caused by injury, biting hard objects, or weakening of the tooth structure
- May expose the sensitive inner layers of the tooth
- Can range from small cracks to complete breaks
Damaged fillings
- Old fillings can wear down, chip, or fall out
- Exposes the previously protected area of the tooth
- Can allow bacteria to enter, potentially leading to decay or infection
Infected tooth pulp (pulpitis)
- Inflammation of the pulp (the tooth’s innermost layer containing nerves and blood vessels)
- Can be caused by deep decay, repeated dental procedures, or trauma
- May require root canal treatment if severe
Tooth abscess
- A pocket of pus caused by bacterial infection
- Can occur at the root tip or in the gums alongside a tooth
- Often results from untreated decay or injury
- Can cause severe pain and potential systemic infection if left untreated
Teeth grinding (bruxism)
- Unconscious clenching or grinding, often during sleep
- Can wear down tooth enamel and cause sensitivity
- May lead to jaw pain and headaches as well
Impacted wisdom teeth
- Occurs when wisdom teeth do not have enough room to emerge properly
- Can cause pain, swelling, and damage to adjacent teeth
- May lead to infection if partially emerged (pericoronitis)
Sensitive teeth
- Can be caused by worn enamel or exposed tooth roots
- Often triggers pain in response to hot, cold, or sweet stimuli
- May result from aggressive brushing, gum recession, or acidic foods
Sinus infection
- Can cause pain in the upper teeth due to pressure in the maxillary sinuses
- Often mistaken for tooth pain, but typically affects multiple upper teeth
Temporomandibular joint (TMJ) disorders
- Problems with the jaw joint can cause pain that feels like it is coming from the teeth
- Often accompanied by jaw clicking, difficulty opening the mouth, or facial pain
How long does a toothache last?
The length of a toothache is dependent on the underlying cause and whether you receive treatment promptly.
Temporary sensitivity
- Can last a few seconds to a few minutes
- Often triggered by hot, cold, or sweet stimuli
- May resolve on its own if caused by minor irritation
Mild tooth decay or gum irritation
- Can persist for several days to weeks
- May come and go or be constant
- Often worsens without treatment
Severe decay or infection
- Can last for weeks or months if untreated
- Pain typically intensifies over time
- Requires professional dental treatment to resolve
Cracked tooth or damaged filling
- Pain may be intermittent or constant
- Can persist indefinitely until treated
- May worsen when biting or chewing
Tooth grinding (bruxism)
- Can cause recurring pain, especially in the morning
- May continue indefinitely if the underlying issue is not addressed
After dental procedures
- Post-treatment sensitivity can last a few days to a few weeks
- Should gradually improve with time
Wisdom tooth emergence
- Can cause intermittent pain for weeks or months as the tooth grows
For persistent toothaches, especially those lasting more than 1-2 days, you should consider being evaluated by a dentist.
Ignoring a toothache can lead to more serious dental issues and potentially longer-lasting pain. Proper diagnosis and treatment can significantly reduce the duration of tooth pain and prevent complications.
Management and Treatment of Toothache
When should I see a dentist for my toothache?
You should see a dentist for your toothache in the following situations:
Persistent pain
- If the pain lasts more than 1-2 days
- Especially if over-the-counter pain relievers do not help
Severe pain
- Intense, throbbing, or unbearable pain
- Pain that interferes with daily activities or sleep
Swelling
- Of the face, jaw, or gums around the affected tooth
- This could indicate an infection or abscess
Fever
- Accompanied by tooth pain, suggesting a possible infection
Difficulty eating or drinking
- Particularly if you are unable to consume hot or cold items
Trauma or injury
- If you have experienced a blow to the tooth or mouth
Loose or knocked-out tooth
- Immediate care can sometimes save the tooth
Signs of infection
- The presence of any bad taste, foul odour, or pus around the tooth
Pain when biting or chewing
- Could indicate a cracked tooth or other serious issues
Persistent sensitivity
- To hot or cold, lasting more than 30 seconds after exposure
Recent dental work
- If you experience severe pain following a dental procedure
Wisdom tooth pain
- Especially if accompanied by swelling or difficulty opening your mouth
Early intervention often leads to simpler, less invasive treatments.
If you are unsure about the severity of your toothache, it is generally better to err on the side of caution and consult a dentist. They can provide a proper diagnosis and recommend appropriate treatment.
When should you go to the ER for a toothache?
While most toothaches can be managed by a dentist, there are situations where seeking emergency medical care is advisable. You should consider going to the ER for a toothache if you are experiencing either one or a combination of the following:
Severe pain: The pain is unbearable and over-the-counter pain medications aren’t helping.
Swelling: There is a build up of fluid or significant swelling in your face or neck, especially if it is affecting your ability to breathe or swallow.
Fever: You have a high fever (over 101°F or 38.3°C) accompanying the toothache, which could indicate a serious infection.
Dental trauma: You have experienced a recent injury to your mouth or face.
Bleeding: There is uncontrolled bleeding from your mouth.
General illness: You are experiencing other symptoms like dizziness, confusion, or chest pain along with the toothache.
Compromised immune system: If you have a weakened immune system (e.g., due to chemotherapy or HIV) and are experiencing severe tooth pain or signs of infection.
After hours: If you are experiencing severe symptoms and the dentist office is closed, you should probably head to an ER.
The ER can manage pain and treat infections, but they typically do not perform dental procedures. They may provide antibiotics and pain relief, and advise you to see a dentist as soon as possible for definitive treatment.
For non-emergency situations, it is usually best to contact your dentist first. Many dental offices have emergency services or can advise you on managing the pain until you can be seen.
How do dentists treat toothaches?
Dentists employ various methods to treat toothaches, tailoring their approach to the specific cause and severity of the pain. The treatment process typically begins with a thorough examination, which may include visual inspection, x-rays, and sensitivity tests to determine the underlying issue.
For minor cases of tooth decay, the dentist might remove the decayed portion of the tooth and fill the cavity with a suitable material such as composite resin or amalgam. If the decay has reached the tooth’s pulp, a root canal procedure might be necessary. This involves removing the infected pulp, cleaning the root canal system, and sealing it to prevent further infection.
In cases where a tooth is severely damaged or infected, extraction may be the best course of action. This is often the case with impacted wisdom teeth that are causing pain and potential harm to adjacent teeth. Following extraction, the dentist might discuss replacement options such as dental implants or bridges.
For toothaches caused by gum disease, the dentist may perform a deep cleaning procedure called scaling and root planing. This involves removing plaque and tartar from below the gum line and smoothing the tooth roots to help the gums reattach to the teeth.
If grinding or clenching is the culprit, the dentist might recommend a custom-fitted night guard to protect the teeth during sleep. For pain related to temporomandibular joint (TMJ) disorders, treatments could range from exercises and lifestyle changes to more advanced interventions like orthodontics or surgery in severe cases.
In some instances, the dentist may prescribe antibiotics to clear up an infection before proceeding with other treatments. They might also recommend over-the-counter or prescription pain relievers to manage discomfort during the healing process.
Specific treatment will depend on the individual case, and the dentist will explain the options and recommend the most appropriate course of action based on their professional assessment.
Toothache medicine
Toothache medicine refers to over-the-counter or prescription medications used to relieve pain caused by tooth decay, gum disease, or other dental issues.
Common over-the-counter options include acetaminophen, ibuprofen, and topical anaesthetics like benzocaine gels. These medications temporarily relieve pain but do not treat the underlying cause, so it is still essential to see a dentist for a proper diagnosis and treatment. In some cases, a dentist might prescribe stronger pain relievers or antibiotics if the toothache is due to an infection.
Dental fillings
Dental fillings are used to repair cavities or small fractures in a tooth caused by decay. The procedure involves removing the decayed portion of the tooth, cleaning the affected area, and then filling it with a material like amalgam, composite resin, porcelain, or gold. Fillings restore the shape and function of the tooth and prevent further decay. Composite resin fillings are popular because they can be matched to the natural colour of your teeth, making them nearly invisible.
Dental crowns
A dental crown is a tooth-shaped cap placed over a damaged, decayed, or weakened tooth to restore its shape, size, strength, and appearance.
Crowns can be made from various materials, including porcelain, ceramic, metal, or a combination of these. The procedure typically requires two visits: one to prepare the tooth and take impressions, and another to place the custom-made crown. Crowns are often used after root canal therapy or to cover a large filling or a dental implant.
Inlays or onlays
Inlays and onlays are types of dental restorations used to repair teeth with moderate decay or damage that is too extensive for a filling but not severe enough to require a crown.
Inlays fit within the cusps (the raised points) of the tooth, while onlays extend over one or more cusps. They are typically made from porcelain, composite resin, or gold. Inlays and onlays are custom-made in a dental lab and are bonded to the tooth, offering a durable and aesthetically pleasing restoration.
Root canal therapy
Root canal therapy is a procedure used to treat infection or inflammation within the pulp of a tooth.
The pulp, which contains nerves and blood vessels, can become infected due to deep decay, repeated dental procedures, or trauma to the tooth.
During a root canal, the dentist removes the infected pulp, cleans and disinfects the inside of the tooth, and fills and seals it to prevent further infection. After the procedure, the tooth is usually restored with a filling or crown to protect it from future damage.
Tooth extraction
Tooth extraction is the removal of a tooth from its socket in the bone. Extractions are performed for various reasons, including severe decay, infection, crowding, or damage that cannot be repaired with a filling or crown. There are two types of extractions: simple and surgical. A simple extraction is performed on a tooth that is visible in the mouth, while a surgical extraction is required for teeth that are not easily accessible, such as impacted wisdom teeth. After an extraction, proper care is necessary to promote healing and prevent complications.
Are there home remedies for toothaches?
Yes there are home remedies for mild to moderate toothaches. However, you should always attempt to visit a dentist as soon as possible when you experience a toothache.
The most common and effective home remedies for toothaches are:
Saltwater rinse
A saltwater rinse is a simple yet effective home remedy for soothing toothache pain and promoting oral health. Saltwater acts as a natural disinfectant, which can help reduce inflammation and cleanse the affected area by flushing out food particles and bacteria.
To use a saltwater rinse, dissolve about half a teaspoon of salt in a cup of warm water. Swish the solution around your mouth for about 30 seconds, making sure to reach the area where you’re experiencing pain. This rinse can also help to reduce swelling and ease discomfort, particularly if the toothache is due to gum irritation or a minor injury.
Hydrogen peroxide rinse
Hydrogen peroxide can be used as a rinse to help alleviate toothache pain and improve oral hygiene. It has antiseptic properties that can kill bacteria and help disinfect the mouth.
To make a hydrogen peroxide rinse, mix equal parts of 3% hydrogen peroxide with water. Swish the solution around your mouth for about 30 seconds before spitting it out. This rinse can be particularly useful if the toothache is associated with an infection or if you have a sore or inflamed area in your mouth.
Do not swallow hydrogen peroxide, as it can be harmful if ingested in large quantities.
Ice packs or cold compress
Applying an ice pack to the outside of your face near the area of pain can help manage a toothache, especially if the pain is accompanied by swelling. The cold temperature helps constrict blood vessels, which can reduce inflammation and numb the area, providing temporary relief from pain.
To use an ice pack, wrap some ice or a frozen gel pack in a cloth to prevent frostbite and apply it to your cheek for 15 to 20 minutes. This can be repeated several times a day as needed to help alleviate discomfort and reduce swelling.
Keep your mouth clean
Maintaining good oral hygiene is crucial for preventing and managing toothaches. Keeping your mouth clean involves brushing your teeth at least twice a day with fluoride toothpaste, flossing daily, and using an antimicrobial mouthwash to reduce bacteria.
Good oral hygiene helps prevent cavities, gum disease, and other issues that can lead to toothaches. If you have an existing toothache, continuing to keep the area clean can help prevent further complications and alleviate some of the pain. Regular dental check-ups are also essential to address any issues before they become severe.
Use over-the-counter pain medication
Over-the-counter (OTC) pain medications can provide temporary relief from toothache pain.
Nonsteroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen, are often recommended because they reduce inflammation and alleviate pain. Acetaminophen is another option, although it does not have anti-inflammatory properties.
Follow the dosing instructions on the packaging and consult with a healthcare provider if you have any health conditions or if the pain persists. OTC pain relievers can help manage discomfort while you wait for a dental appointment or until you address the underlying issue.
Avoid foods or drinks with extreme temperatures
Foods and drinks that are very hot or very cold can trigger or worsen toothache pain, especially if your teeth are sensitive or if there is existing damage. Extreme temperatures can cause discomfort by stimulating the nerve endings in your teeth.
To prevent exacerbating your toothache, try to avoid consuming very hot or cold foods and beverages. Opt for foods and drinks at a moderate temperature and consider consuming softer foods that are less likely to irritate the affected area. This can help minimise discomfort and prevent additional pain while you seek professional dental care.
How can toothaches be prevented?
Preventing toothaches involves a combination of good oral hygiene practices, lifestyle choices, and regular dental care.
Maintaining a consistent oral hygiene routine is crucial. Brushing your teeth at least twice a day with fluoride toothpaste helps remove plaque and prevent cavities, which are a common cause of toothaches. Flossing daily is equally important, as it removes food particles and plaque from between the teeth and under the gumline, where a toothbrush might not reach.
Regular visits to the dentist for check-ups and cleanings play a key role in preventing toothaches. Dentists can detect early signs of problems such as cavities, gum disease, or cracks before they become severe, providing timely treatment to prevent pain. They can also offer professional cleanings to remove tartar build-up that can lead to decay and gum issues.
Dietary choices also impact dental health. Reducing your intake of sugary and acidic foods and beverages can help prevent cavities. Sugars and acids contribute to plaque formation and can erode enamel, increasing the risk of tooth decay and sensitivity. Additionally, drinking plenty of water helps wash away food particles and bacteria that can cause tooth decay.
Protecting your teeth from physical damage is another preventive measure. If you engage in activities that carry a risk of dental injury, such as sports, wearing a mouthguard can help protect your teeth from impact and trauma. This is particularly important for those with braces or other dental appliances.
Avoiding habits like using your teeth as tools to open packages or chewing on hard objects that help prevent the potential for cracks or damage to your teeth.Smoking and chewing tobacco are harmful to oral health as well, contributing to gum disease and tooth decay.
The best way to prevent toothaches is to address any issues promptly when they arise. If you notice any signs of tooth sensitivity, pain, or changes in your oral health, seeking dental care right away can help prevent more serious problems from developing. By combining these preventive strategies, you can significantly reduce your risk of toothaches and maintain better overall dental health.
Toothache: Frequently Asked Questions
Why does my tooth hurt when I bite down on it?
If your tooth hurts when you bite down on it, there are several potential reasons for this discomfort.
One common cause is that the filling or dental work you recently had done might be too high or uneven, causing your bite to be off. When you bite down, the pressure can put stress on the tooth and surrounding structures, leading to pain.
Another possibility is that the tooth might have underlying issues such as a crack or a small fracture that wasn’t detected before the filling was placed. These cracks can become more pronounced under the pressure of chewing, causing pain.
Sometimes, the pain is due to inflammation or irritation of the nerve of the tooth, particularly if the filling was deep or if the cavity was close to the nerve. This irritation can make the tooth sensitive to pressure.
If you have recently had a crown placed, it could be that the crown has not been fitted well, or that the tooth underneath is still reacting to the new structure. In some cases, the pain might also be related to issues like gum inflammation or an infection that’s affecting the tooth and surrounding tissues.
If the pain persists, consult with your dentist to determine the exact cause and to find a solution. They can assess the bite, examine the tooth, and check for any potential problems with the filling or other dental work.
Why does my tooth hurt when I drink something cold?
Experiencing pain when drinking something cold can be quite uncomfortable and is often a sign that something is amiss with your tooth or dental health. This sensitivity is usually due to a few possible reasons.
One common cause is that the enamel of the tooth, which serves as a protective layer, may be worn down or damaged. Enamel erosion exposes the dentin, the layer underneath the enamel that contains tiny nerve endings. When you consume something cold, the temperature change can directly affect these nerves, leading to sharp or lingering pain.
Another possibility is that you might have a cavity or decay in the tooth. Cavities create small holes or weak spots in the tooth that can allow cold temperatures to reach the nerve endings inside the tooth, causing pain when you eat or drink something cold.
Sometimes, a recent dental treatment such as a filling or crown might lead to temporary sensitivity, especially if the tooth was treated for issues close to the nerve. This sensitivity can make the tooth react to cold temperatures more intensely until it adjusts or heals.
Gum recession is another factor that can contribute to sensitivity. When the gums pull back from the tooth, they expose the root surface, which is more sensitive to temperature changes than the enamel. Drinking something cold can then trigger discomfort or pain in these areas.
If the pain is persistent or severe, do consult your dentist. They can help diagnose the underlying cause of your sensitivity and recommend appropriate treatment or preventive measures to alleviate your discomfort.
Can a toothache go away on its own?
A toothache might sometimes subside on its own, but this is not always a reliable or advisable outcome.
In some cases, the pain could diminish if the underlying issue is minor or temporary. For example, if the pain is due to something like a bit of food trapped between the teeth or minor gum irritation, it might go away once the irritant is removed or the gum heals.
However, if the toothache is caused by something more serious, such as tooth decay, an infection, or a crack in the tooth, it is unlikely to resolve without professional treatment.
Infections or severe decay typically require dental intervention to address the underlying problem effectively. Ignoring a toothache, especially if it persists or worsens, can lead to more serious complications like abscesses, tooth loss, or systemic infections.
Even if the pain does go away, you should visit a dentist to determine the cause and ensure that no significant damage or disease is present. A dentist can assess the situation, provide appropriate treatment, and help prevent future issues. So while a toothache might temporarily improve on its own, it is generally best to seek dental advice to address any potential underlying problems and to maintain overall oral health.
What is the best painkiller for toothache?
The best painkiller for a toothache largely depends on your individual needs and any specific health considerations you might have. Generally, over-the-counter (OTC) pain relievers can be effective for managing toothache discomfort.
Nonsteroidal anti-inflammatory drugs (NSAIDs) like ibuprofen are often recommended because they not only relieve pain but also reduce inflammation, which can be particularly helpful if the toothache is due to inflammation or an infection. Ibuprofen can be taken in standard doses as directed on the package.
Acetaminophen is another option that can help with pain relief, especially if you are unable to take NSAIDs due to allergies, stomach issues, or other health concerns. While acetaminophen doesn’t have anti-inflammatory properties, it can still be effective in managing pain.
For individuals who cannot tolerate OTC painkillers or have specific health conditions, a dentist might prescribe stronger medications or provide alternative pain management strategies. It is always important to follow the dosing instructions carefully and to consult with a healthcare provider or dentist if you have any underlying health issues or if the pain persists despite medication.
While painkillers can provide temporary relief, they do not address the underlying cause of the toothache. The best way to treat a toothache is to see a dentist to diagnose and treat the root of the problem to prevent further complications.
How can you tell what kind of toothache you have?
Determining the type of toothache you have often involves paying close attention to the nature of the pain, its location, and any associated symptoms. The characteristics of your toothache can provide clues about its underlying cause.
For instance, if you are experiencing sharp and sudden pain when you eat or drink something hot or cold, it might indicate that the enamel of the tooth is worn down or that the tooth has a cavity close to the nerve. This type of pain usually results from sensitivity due to exposure of the inner layers of the tooth.
A constant, throbbing pain, especially if it is severe and persistent, can be a sign of an infection or abscess. Infections typically cause significant discomfort and may be accompanied by swelling, fever, or a bad taste in the mouth. The pain can be widespread, affecting not just the tooth but also the surrounding areas like the jaw or neck.
If the pain is localised to a specific tooth and is accompanied by discomfort when you apply pressure or chew, it could indicate issues such as a cracked tooth or dental filling. A cracked tooth might cause intermittent pain, particularly when biting down, and might be more noticeable when chewing certain types of food.
Gum issues, such as gum disease or gingivitis, can also cause pain, often accompanied by symptoms like bleeding, swelling, or bad breath. This pain typically affects the gum line around the tooth rather than the tooth itself.
In some cases, pain can radiate from other areas, such as sinus infections, which might cause discomfort in the upper teeth due to their proximity to the sinus cavities. Sinus-related pain often feels like a dull ache or pressure rather than sharp tooth pain.
While these observations can provide some insight, a thorough examination by a dentist is essential for an accurate diagnosis. They can perform tests, such as X-rays or thermal sensitivity tests, to pinpoint the exact cause of the pain and recommend appropriate treatment.
Make An Enquiry
Let us know your concerns and our clinic staff will get back to you in 1-2 hours.
Prefer to talk to our clinic staff directly? Call our clinic to chat with our friendly nurses at +65 6767 9502
General Information
-
Yew Tee Point
21 Choa Chu Kang North 6 #01-27 Singapore 689578
Tel: +65 6767 9502
(Please Enter The Clinic From Outside The Mall) -
Consulting Hours
Mon to Fri: 9AM to 9PM
Sat: 9AM to 6PM
Sun and PH: Closed
Related Articles
-

10 Effective Ways To Treat Gingivitis At Home
If you suspect that you have gum disease or have recently been diagnosed with early-stage gum disease (gingivitis), you might be wondering whether there is...
Read More -

5 Early Warning Signs of Gum Disease You Shouldn’t Ignore
How do you know if you have gum disease? As a dentist who has helped treat many patients suffering from various stages of gum disease,...
Read More -

6 Signs You Should Visit A Periodontist for Gum Disease Treatment
You might be aware that a periodontist is a gum specialist doctor who treats gum conditions. You might also suspect that you are suffering from...
Read More -

Can I Use Medisave For Gum Disease Treatment?
Patients who visit Kong Dental Surgery often ask us about the available financing options we have. One of the most common questions that we receive...
Read More -
Does Osteoporosis Affect Your Teeth?
Osteoporosis does affect your teeth. People with osteoporosis are at a higher risk of tooth loss. This is because of the lower bone mineral...
Read More


