Tooth Decay: Symptoms, Causes and Treatment
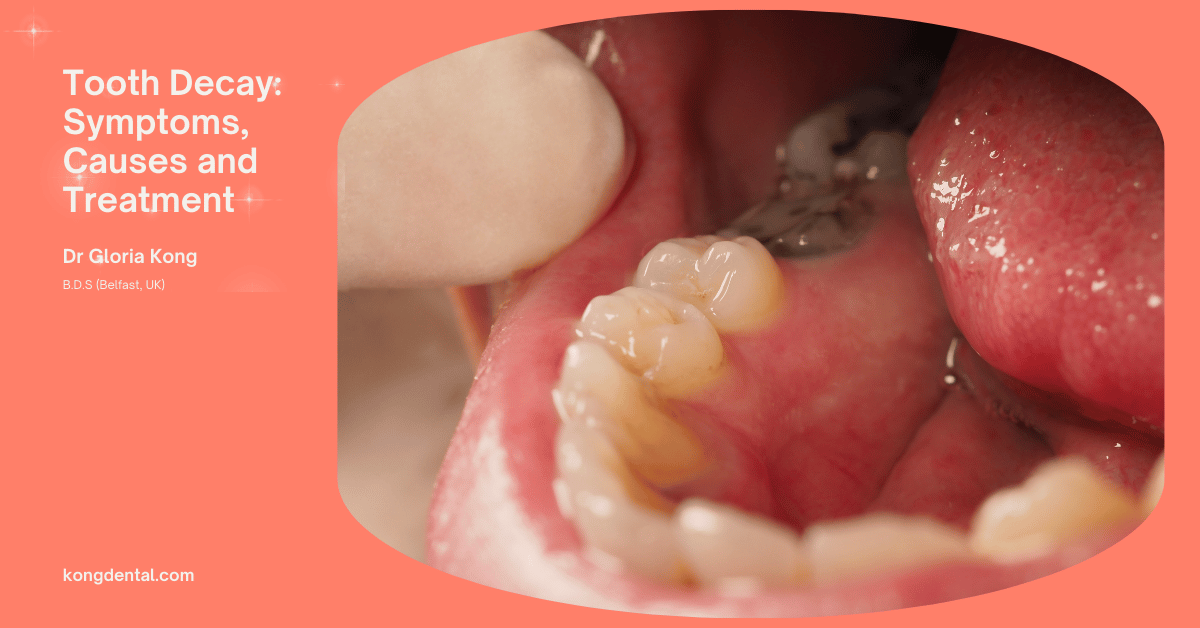
Tooth decay is a silent and ticking time bomb. It can occur without causing any pain or discomfort in the initial stages. You might refer to it as a “hole in your tooth” or a tooth cavity.
Whatever the term used, tooth decay can lead to pain and costly dental procedures if left untreated.
What is Tooth Decay?
Tooth decay, also known as dental caries or cavities, is a common oral health problem. It occurs when bacteria in the mouth produce acids that erode tooth enamel, the hard protective outer layer of teeth.
These bacteria thrive on sugars and starches from food particles left on teeth, forming a sticky film called plaque. As the acids continue to attack the enamel, they create small holes or cavities in the tooth structure.
If left untreated, tooth decay can progress deeper into the tooth, affecting the softer dentin layer and eventually reaching the pulp, which contains nerves and blood vessels. This can lead to pain, infection, and potential tooth loss.
Tooth decay is preventable through good oral hygiene practices, such as regular brushing and flossing, a balanced diet low in sugary foods, and routine dental check-ups. Fluoride treatments and dental sealants can also help protect teeth from decay. Early detection and treatment of tooth decay can prevent more serious dental problems and maintain overall oral health.
What is Cavity?
A cavity is a hole that forms in a tooth due to tooth decay. It occurs when bacteria in the mouth produce acid that erodes the tooth’s enamel and underlying layers.
As the decay progresses, it creates a small hole or pit in the tooth, which is the cavity.
Cavities can vary in size and depth, ranging from minor surface damage to deep holes that reach the tooth’s inner pulp. If left untreated, cavities can cause pain, infection, and eventual tooth loss.
They are typically treated by removing the decayed portion of the tooth and filling the hole with a dental material.
Regular dental hygiene, including brushing, flossing, and dental check-ups, helps prevent cavities by removing plaque and bacteria before they can cause significant damage to the tooth structure.
Types of Tooth Decay
There are several different classifications based on the location and progression of the decay:
Pit and fissure decay
Occurs on the chewing surfaces of the back teeth. These areas have deep grooves and crevices where bacteria can easily accumulate, making them prone to decay.
Smooth surface decay
Typically affects the flat outer surfaces of teeth, often between teeth where brushing and flossing may be less effective.
Root decay
Occurs on the exposed roots of teeth, usually in older adults who have receding gums. The roots lack protective enamel, making them more vulnerable to decay.
Recurrent decay
Happens around existing fillings and crowns. These areas can be more susceptible to new decay if not properly maintained.
Early childhood caries (Baby bottle tooth decay)
Affects infants and young children, often due to prolonged exposure to sugary liquids.
Interproximal decay
Develops between teeth where they touch each other, making it difficult to clean these areas effectively with regular brushing alone.
How common are dental cavities?
Dental cavities are extremely common, making them one of the most prevalent chronic diseases worldwide.
They affect people of all ages, from young children to older adults. In fact, most people will experience at least one cavity in their lifetime.
The World Health Organization estimates that nearly 100% of adults have dental cavities, while approximately 60-90% of school-age children are affected.
The prevalence of cavities varies by region, socioeconomic status, and access to dental care, with higher rates often seen in low-income areas and developing countries.
Despite improvements in dental hygiene practices and fluoridation efforts, cavities remain a significant public health concern. Their widespread occurrence underscores the importance of regular dental check-ups, proper oral hygiene, and preventive measures to maintain good oral health throughout your life.
Who can get tooth decay?
Tooth decay can affect anyone. This is regardless of age, gender, or background. It is a universal dental problem that can occur throughout the lifetime of a person.
Children are particularly susceptible to tooth decay due to their diet, developing oral hygiene habits, and the fact that their tooth enamel is still maturing. However, adults are not immune and can develop cavities at any age, especially as gums recede and expose more vulnerable parts of the teeth.
Older adults face an increased risk as they may have dry mouth from medications or medical conditions, making them more prone to decay. People with poor oral hygiene, diets high in sugar and carbohydrates, or limited access to dental care are at higher risk.
Additionally, individuals with certain medical conditions, such as diabetes or autoimmune disorders, may be more susceptible to tooth decay.
Even those who maintain good oral health practices can develop cavities, as factors like genetics, tooth shape, and saliva composition also play a role. Essentially, tooth decay is a potential concern for everyone, highlighting the importance of consistent dental care and preventive measures throughout life.
Symptoms and Causes of Tooth Decay
Tooth decay typically develops gradually and may not cause noticeable symptoms in its early stages. As the decay progresses, symptoms can include:
Toothache or pain, which may be spontaneous or occur when eating or drinking, especially sweet, hot, or cold items. Sensitivity to temperature changes in food or drinks. Visible holes or pits in the teeth. Brown, black, or white staining on the surface of a tooth. Pain when biting down or chewing. In advanced stages, swelling of the gum around the affected tooth or facial swelling may occur.
The primary cause of tooth decay is the interaction between bacteria in the mouth and sugars from food. Bacteria form a sticky film called plaque on teeth, and when you consume sugary or starchy foods, these bacteria feed on the sugars, producing acid as a byproduct. This acid attacks the tooth enamel, gradually breaking it down and leading to decay.
What causes cavities?
There are many causes.
- Poor oral hygiene, which allows plaque to build up.
- A diet high in sugary and starchy foods and drinks.
- Frequent snacking, which provides constant fuel for acid-producing bacteria.
- Dry mouth, as saliva, helps neutralise acids and wash away food particles.
- Lack of fluoride, which helps strengthen tooth enamel.
- Genetics, which can influence the strength of tooth enamel and susceptibility to decay.
- Medical conditions that affect oral health, such as diabetes or acid reflux.
- Certain medications that reduce saliva production.
Understanding these symptoms and causes is crucial for early detection and prevention of tooth decay. Regular dental check-ups can help identify decay before it becomes severe, allowing for timely treatment and preservation of oral health.
What are the signs of cavities?
The signs of cavities can vary depending on their location and severity, but often develop gradually.
Early-stage cavities may not cause any noticeable symptoms, which is why regular dental check-ups are crucial for detection. As decay progresses, common signs include tooth sensitivity, especially to hot, cold, or sweet foods and drinks. This sensitivity may initially be mild but can become more persistent or intense over time.
Visible changes to the tooth surface can also indicate cavities. These may appear as white spots on the enamel, which can darken to brown or black as the decay advances. Small holes or pits in the teeth, visible to the naked eye or felt with the tongue, are clear signs of cavity formation.
In more advanced stages, you might experience a toothache or pain when biting down, which can range from mild discomfort to severe, constant pain.
Bad breath or an unpleasant taste in the mouth can also be symptoms of decay, especially if they persist despite good oral hygiene. In some cases, you might notice swelling or tenderness in the gums near the affected tooth. As cavities worsen, they can lead to more serious complications like infections, resulting in facial swelling or fever.
However, not all cavities cause pain or visible symptoms, especially in their early stages. This is why dentists often use X-rays and other diagnostic tools to detect cavities before they become more serious. If you notice any of these signs or have concerns about your dental health, do seek assistance from a dental clinic.
Tooth decay stages
Tooth decay, also known as dental caries, is a progressive disease that can lead to serious oral health problems if left untreated. It typically progresses through several stages:
- Initial Attack: Bacteria in the mouth produce acids that erode the tooth enamel.
- White Spot Stage: A small, white spot may appear on the tooth surface. This indicates that the enamel has been weakened.
- Cavity Formation: As the decay progresses, a cavity or hole forms in the tooth.
- Pulp Involvement: The decay may reach the pulp, the soft, inner part of the tooth that contains nerves and blood vessels. This can cause severe pain and infection.
- Tooth Abscess: If the infection spreads to the surrounding tissues, a tooth abscess may form. This can cause pain, swelling, and sensitivity.
- Tooth Loss: In severe cases, the tooth may become so damaged that it needs to be extracted.
These stages are not always linear. The progression of tooth decay can vary depending on factors such as diet, oral hygiene, and genetics.
If you notice any signs of tooth decay, such as pain, sensitivity, or discoloration, the best advice is to see a dentist as soon as possible. Early detection and treatment can help prevent more serious complications.
What are the risk factors for cavities?
Several factors can increase your risk of developing cavities:
- Poor oral hygiene: Brushing your teeth twice a day, flossing daily, and seeing your dentist for regular check-ups are essential for preventing cavities.
- Diet: Consuming sugary and starchy foods and drinks can contribute to tooth decay.
- Dry mouth: Saliva helps to neutralise acids in the mouth and protect teeth from decay. People with dry mouth may be at a higher risk for cavities.
- Certain medications: Some medications can reduce saliva production or cause dry mouth, increasing the risk of cavities.
- Genetics: Some people may be more susceptible to cavities due to genetic factors.
- Acid reflux: Acid reflux can erode the enamel on your teeth, making them more susceptible to decay.
- Chewing tobacco: Tobacco use can damage the teeth and gums, increasing the risk of cavities.
By addressing these risk factors and practising good oral hygiene, you can significantly reduce your chances of developing cavities.
Are cavities contagious?
No, cavities are not contagious. They are caused by bacteria that live in your mouth, not by germs that are transmitted from person to person.
While the bacteria that cause cavities can be shared through close contact, such as kissing or sharing utensils, the actual cavities themselves are not contagious.
Diagnosis and Tests for Tooth Decay
How are cavities diagnosed?
Dentists use a combination of visual examination, special tools, and X-rays to diagnose dental decay.
At Kong Dental, we use the following steps to find out whether you have dental cavities:
- Visual Examination: The dentist will carefully examine your teeth, looking for signs of decay such as dark spots, pits, or discoloration.
- Dental Explorer: This is a thin, metal tool that the dentist uses to probe the tooth’s surface for soft spots or cavities.
- Bitewing X-rays: These X-rays provide a side view of your teeth and jaw, allowing the dentist to see cavities between your teeth.
- Panoramic X-rays: In some cases, panoramic X-rays may be used to get a full view of your teeth and jawbone.
Tooth Decay Complications
If left untreated, tooth decay can lead to several serious complications:
- Tooth Abscess: This is a painful infection that occurs when bacteria invade the pulp (the soft, inner part of the tooth). It can cause severe pain, swelling, and sensitivity.
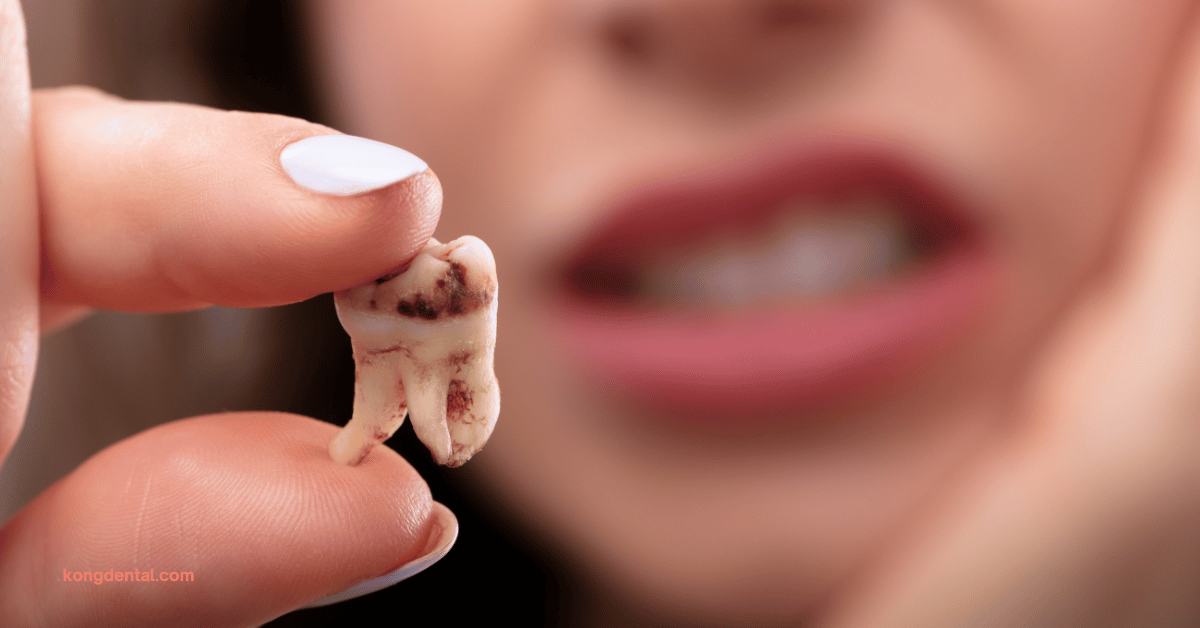
- Tooth Loss: If the infection spreads or the tooth becomes too damaged, it may need to be extracted.
- Jawbone Infection: In severe cases, the infection can spread to the jawbone, causing pain, swelling, and difficulty opening your mouth.
- Systemic Infection: In rare cases, a tooth infection can spread to other parts of the body, causing a systemic infection.
Management and Treatment of Tooth Decay
How do you get rid of cavities?
The only way to get rid of cavities is to see a dentist. They can assess the severity of the decay and recommend the appropriate treatment.
Address cavities promptly to prevent further complications. Delaying treatment can lead to more severe pain, infection, and even tooth loss.
How Dental Treatments Treat Tooth Decay
Fluoride
Fluoride strengthens tooth enamel, making it more resistant to acid attacks from bacteria.
Usage: Fluoride is found in toothpaste, mouthwash, and dental treatments. It can also be applied directly to teeth in the form of fluoride varnishes or gels.
Benefits: Fluoride helps prevent cavities and can even reverse early stages of decay.
Dental Fillings
Fillings are used to repair cavities by removing the decayed portion of the tooth and replacing it with a restorative material.
Usage: Fillings can be made from various materials, including composite resin, amalgam, and glass ionomer cement. They are applied to the cavity and shaped to match the surrounding tooth structure.
Benefits: Fillings restore the function and appearance of the tooth, preventing further decay and pain.
Root Canal Therapy
When decay reaches the pulp (the soft, inner part of the tooth), root canal therapy is used to remove the infected pulp and seal the tooth to prevent further infection.
Usage: The dentist drills a small hole in the tooth, removes the infected pulp, and fills the root canals with a special material. The tooth is then sealed with a crown or filling.
Benefits: Root canal therapy can save a severely decayed tooth, preventing the need for extraction and preserving the natural tooth structure.
Tooth Extraction
Tooth extraction is the removal of a tooth from the jawbone.
Usage: Extraction is typically used when a tooth is severely decayed, damaged, or infected beyond repair. It may also be necessary for orthodontic reasons or to prevent the spread of infection.
Benefits: Extraction can relieve pain and prevent the spread of infection. However, it is important to note that tooth extraction can have long-term consequences, such as changes in bite and facial structure.
Prevention of Tooth Decay
How can I prevent cavities?
Here are some tips to help prevent cavities:
- Brush your teeth twice a day with a fluoride toothpaste.
- Floss daily to remove food particles and plaque from between your teeth.
- See your dentist for regular check-ups and cleanings.
- Limit your intake of sugary and starchy foods and drinks.
- Drink plenty of water.
- Consider using a mouthwash with fluoride.
- Do not smoke or chew tobacco.
- If you have dry mouth, talk to your dentist about ways to increase saliva production.
- Use a fluoride toothpaste and mouthwash.
- Chew sugarless gum.
What Can I Expect if I Have Cavities?
If you have cavities, you may experience the following symptoms:
- Pain or sensitivity to hot, cold, sweet, or acidic foods and drinks
- Dark spots or pits on the surface of your teeth
- Discoloration of your teeth
- Bad breath or a foul taste in your mouth
- Swelling or tenderness around your teeth or gums
In severe cases, you may also experience:
- Tooth abscess: A painful infection that can cause swelling and sensitivity.
- Tooth loss: If the decay is severe, the tooth may need to be extracted.
It’s important to see a dentist as soon as you notice any of these symptoms. Early treatment can help prevent more serious complications and save your natural teeth.
Your dentist will be able to diagnose your cavities and recommend the appropriate treatment.
With proper treatment, you can effectively manage cavities and maintain good oral health.
When Should I Call a Dentist About My Tooth Decay?
You should call a dentist as soon as you notice any signs of tooth decay. These signs can include:
- Pain or sensitivity to hot, cold, sweet, or acidic foods and drinks
- Dark spots or pits on the surface of your teeth
- Discoloration of your teeth
- Bad breath or a foul taste in your mouth
- Swelling or tenderness around your teeth or gums
Even if you are not experiencing any symptoms, it’s a good idea to see a dentist for regular check-ups. Early detection and treatment can help prevent more serious problems.
Don’t delay seeking dental care. The sooner you address tooth decay, the better the chances of preserving your natural tooth.
What questions should I ask my dentist about my tooth decay?
Here are some questions you might want to ask your dentist about your tooth decay:
- What is the extent of the decay? This will help you understand the severity of the problem and the possible treatment options.
- What are the treatment options available? Your dentist can explain the different procedures that could be used to address your tooth decay.
- What are the risks and benefits of each treatment option? This will help you make an informed decision about your care.
- What are the expected costs of the treatment? Knowing the costs involved can help you plan your budget accordingly.
- How long will the treatment take? This will give you an idea of the time commitment required.
- What can I expect during and after the treatment? This will help you prepare for the procedure and understand what to expect in terms of recovery.
- How can I prevent future tooth decay? Your dentist can provide you with tips on maintaining good oral hygiene and avoiding factors that contribute to tooth decay.
Tooth Decay: Frequently Asked Questions
What does a cavity look like?
Cavities can be difficult to see on your own, especially in their early stages. They often appear as small, dark spots or pits in the tooth enamel. However, as the decay progresses, they may become more noticeable and may even cause pain or sensitivity.
Here are some visual cues to look for:
- Dark spots or pits: These can be seen on the surface of the tooth.
- Discoloration: The affected area may appear darker or more yellow than the surrounding teeth.
- Sensitivity: You may experience sensitivity to hot or cold temperatures, or to sweet or acidic foods and drinks.
- Pain: As the cavity deepens, it can cause pain, especially when chewing.
If you suspect you may have a cavity, do see a dentist for a professional examination. They can use special tools and techniques to detect and diagnose cavities, even in their early stages.
What is the difference between a cavity vs a stain?
Cavities and stains are both dental issues, but they are different in nature and severity.
Cavities are essentially holes in the tooth enamel caused by bacterial decay. This decay occurs when bacteria feed on sugars and starches in the mouth, producing acids that erode the enamel. Cavities can cause pain, sensitivity, and even tooth loss if left untreated.
Stains are discolorations on the teeth that can be caused by various factors, including:
- Food and drink: Certain foods and drinks, such as coffee, tea, red wine, and soda, can stain teeth.
- Tobacco: Smoking or chewing tobacco can stain teeth yellow or brown.
- Medications: Some medications can cause tooth discoloration as a side effect.
- Poor oral hygiene: Plaque and tartar buildup can contribute to tooth stains.
While stains can be unsightly, they are generally not harmful to the teeth. However, they can be difficult to remove and may require professional teeth whitening treatments.
If you are concerned about the appearance of your teeth, consult with a dentist. They can help you determine whether you have cavities or stains and recommend the appropriate treatment.
What happens if you have a cavity for a long time?
If a cavity is left untreated for a long time, it can lead to several serious complications:
- Tooth Abscess: This is a painful infection that occurs when bacteria invade the pulp (the soft, inner part of the tooth). It can cause severe pain, swelling, and sensitivity.
- Tooth Loss: If the infection spreads or the tooth becomes too damaged, it may need to be extracted. This can lead to the need for dentures or dental implants.
- Jawbone Infection: In severe cases, the infection can spread to the jawbone, causing pain, swelling, and difficulty opening your mouth.
- Systemic Infection: In rare cases, a tooth infection can spread to other parts of the body, causing a systemic infection.
You should try to visit a dentist as soon as you notice any signs of a cavity. Early treatment can often prevent these dental complications and save your natural tooth.
Can a cavity heal on its own?
No, a cavity cannot heal on its own. Once decay has started, it will continue to progress if left untreated. The bacteria that cause cavities will continue to erode the tooth enamel, leading to more significant damage over time.
Seek professional dental care as soon as you notice any signs of a cavity. A dentist can assess the severity of the decay and recommend the appropriate treatment, which may include:
- Dental filling: For minor cavities, a dentist can remove the decayed portion and fill the cavity with a material like composite resin or amalgam.
- Crown: If a significant portion of the tooth is decayed, a crown can be placed over the remaining tooth structure to restore its shape and function.
- Root canal treatment: If the decay has reached the tooth's pulp (the soft, inner part), a root canal may be necessary. This procedure involves removing the infected pulp and sealing the tooth to prevent further infection.
Delaying treatment can lead to more severe complications, such as tooth abscess, tooth loss, or even infection that spreads to other parts of the body.
Can decaying teeth be restored?
Yes, decaying teeth can often be restored. The treatment method depends on the severity of the decay.
Here are some common treatments:
- Dental filling: For minor decay, a dentist can remove the decayed portion and fill the cavity with a material like composite resin or amalgam.
- Dental crown: If a significant portion of the tooth is decayed, a crown can be placed over the remaining tooth structure to restore its shape and function.
- Root canal treatment: If the decay has reached the pulp of your tooth (the soft, inner part), a root canal may be necessary. This procedure involves removing the infected pulp and sealing the tooth to prevent further infection.
The earlier you address tooth decay, the better the chances of restoring your tooth.
Delaying treatment can lead to more severe complications, such as tooth abscess or tooth loss. If you notice any signs of tooth decay, such as pain, sensitivity, or discoloration, please consider calling a dentist for an appointment immediately.
If a cavity hurts, is it too late?
It depends what you mean by too late. If this is in reference to a tooth extraction, then no, it might not necessarily be too late to save your tooth, even if it has been causing you pain.
While it is best to address cavities early to prevent further damage, a dentist can often treat a painful cavity.
However, the sooner you seek treatment, the better the chances of preserving your natural tooth. Delaying treatment can lead to more severe complications, such as:
- Tooth abscess: A pocket of pus that forms at the root of the tooth, causing severe pain and swelling.
- Tooth loss: If the infection spreads or the tooth becomes too damaged, it may need to be extracted.
If you are experiencing tooth pain, it is generally a good idea to visit a dentist as soon as possible. They can assess the severity of the cavity and recommend the appropriate treatment, which may include:
- Dental filling: A procedure to repair the cavity and prevent further decay.
- Root canal treatment: A treatment to remove the infected pulp inside the tooth and seal it to prevent future infection.
- Tooth extraction: In severe cases, the tooth may need to be removed.
Make an appointment with your dentist. Early intervention can often save your tooth and prevent more serious problems.
Make An Enquiry
Let us know your concerns and our clinic staff will get back to you in 1-2 hours.
Prefer to talk to our clinic staff directly? Call our clinic to chat with our friendly nurses at +65 6767 9502
General Information
-
Yew Tee Point
21 Choa Chu Kang North 6 #01-27 Singapore 689578
Tel: +65 6767 9502
(Please Enter The Clinic From Outside The Mall) -
Consulting Hours
Mon to Fri: 9AM to 9PM
Sat: 9AM to 6PM
Sun and PH: Closed
Related Articles
-

5 Early Warning Signs of Gum Disease You Shouldn’t Ignore
How do you know if you have gum disease? As a dentist who has helped treat many patients suffering from various stages of gum disease,...
Read More -

How Often Do You Need To See A Dentist?
We all know that keeping our teeth healthy and clean cannot be overlooked. Moreover, our oral health is closely related to our overall health.1 After...
Read More -

Pain Free Dentistry: Is There A Pain Free Dental Clinic in Singapore?
For many individuals, dental procedures are often associated with pain and discomfort. You might be one of them too. Fear of pain often deters patients...
Read More -

Tooth Discolouration (Stained Teeth): Causes, Prevention and Treatment
What is Tooth Discolouration? Tooth discoloration occurs when the colour of your teeth changes. This colour change makes your teeth appear less bright or white...
Read More -
Toothache: Causes, Treatment and Prevention
A toothache can cause significant discomfort to you. It can even impede you from going about with your day normally. A toothache can also be...
Read More


